
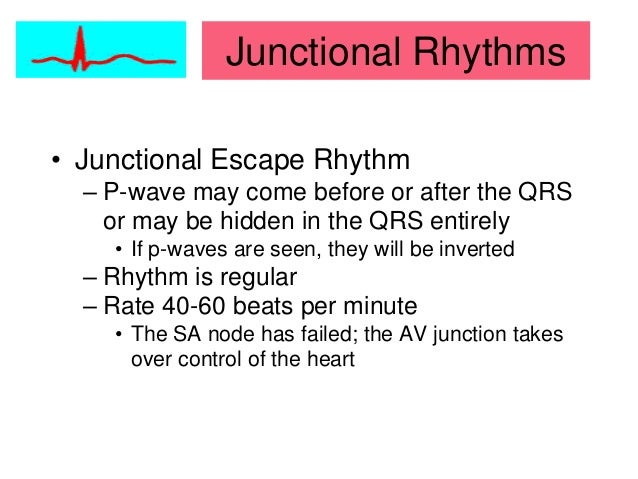
Latent pacemakers can continue discharging impulses until the sinoatrial node recovers and starts discharging. Also note the ST-segment elevations (which in this case has no relation to the sinoatrial arrest).Īs discussed in Chapter 1, if the sinoatrial node fails to discharge an impulse, there are three latent pacemaker structures that can (and will) discharge impulses that will salvage the situation. Part 8: Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Diagnostic criteria of broad QRS complex tachycardia: decades of evolution. Consider adenosine as an initial therapy for an undifferentiated wide complex tachycardiaĪlzand BCrijns H.Unstable WCT requires immediate synchronized cardioversion (when the symptoms are believed to be due to the heart rhythm).Obtain a 12-lead ECG before and after treatment to help aid in the diagnosis.Wide complex tachycardias should be presumed to be VT until proven otherwise.In many cases it can be considered as a first line therapy for undifferentiated wide complex tachycardia, and may have some diagnostic utility when considered in the context of other findings. Retrospectively, adenosine would have been safe and likely effective. It is safe to conclude that this patient had a conduction defect at baseline, which is what caused the complexes to be wide during the tachycardia. The axis and QRS morphology are noted to be exactly the same. Once the patient converts to sinus tachycardia (and after a sigh of relief) paramedics compare the two 12-lead ECGs. She is placed on the cardiac monitor and the following rhythm strip is obtained.įigure 3: Now there is sinus tachycardia with virtually identical QRS morphology. Radial pulses are very rapid but surprisingly strong. On initial assessment the patient is found to be alert and oriented to person, place, time, and event. Past medical history includes myocardial infarction and hypertension. See also: Myths and Cognitive Biases in Interpretation of Wide Complex TachycardiasĮMS is dispatched to an 83-year-old female who contacts 9-1-1 after she wakes up with a “racing heart” and shortness of breath. There are good criteria to help rule-in, or tip the scales in favor of VT, but none to safely rule-out VT. In particular, treating a wide complex tachycardia with a calcium channel blocker is a dangerous decision that could have fatal consequences for your patient. The short answer is yes, but it can be very difficult, and even experienced clinicians can misdiagnose VT as SVT with aberrancy! When a patient with a bundle branch block experiences SVT the result is a wide complex tachycardia.Ĭan you differentiate between SVT with aberrant conduction and VT? Additionally, we know that many patients have underlying bundle branch block, including bifascicular block, at baseline. When something is aberrant it “departs from the right, normal, or usual course.”īecause the right bundle branch tends to have a slightly longer refractory period than the left bundle branch, at higher rates the right bundle branch may not be fully recovered from the previous cardiac cycle, which results in a right bundle branch block pattern.Įven though right bundle branch block aberrancy is more common than left bundle branch block aberrancy, both are possible. You can think of “aberrancy” as abnormal conduction. It is usually treated with vagal maneuvers or adenosine. This arrhythmia is usually stable and the prognosis is much more favorable than VT.
What most people really mean when they call a rhythm “SVT” is AV Nodal Reentrant Tachycardia or AVNRT, which is a reentrant rhythm in or around the AV node. A good rule of thumb to estimate the maximum sinus rate is 220 minus age but that can vary by 10-15%, which is a lot. In reality, sinus tachycardia is a form of SVT, and the rate can easily exceed 150. This is important because many of us were taught a narrow complex rhythm “must be SVT if the rate is over 150,” which can lead to inappropriate therapies. In this guideline, the term does not include AF.” These SVTs include inappropriate sinus tachycardia, AT (including focal and multifocal AT), macroreentrant AT (including typical atrial flutter), junctional tachycardia, AVNRT, and various forms of accessory pathway-mediated reentrant tachycardias. “An umbrella term used to describe tachycardias (atrial and/or ventricular rates in excess of 100 bpm at rest), the mechanism of which involves tissue from the His bundle or above. The term “SVT with aberrancy” tends to throw many providers off so let’s start by defining SVT using the 2015 ACC/AHA/HRS Guidelines as reference.


 0 kommentar(er)
0 kommentar(er)
